WV Computerized Patient Record System CPRS
Porting VistA to the OLPC. For introduction to VistA components see VistA Monograph Wiki.
Computerized Patient Record System (CPRS)
Status
![]() Check
Check
![]() Alt CPRS Alternative OpenVista CIS
Alt CPRS Alternative OpenVista CIS
Porting to OLPC XO
There are several options for Porting Clients to the XO
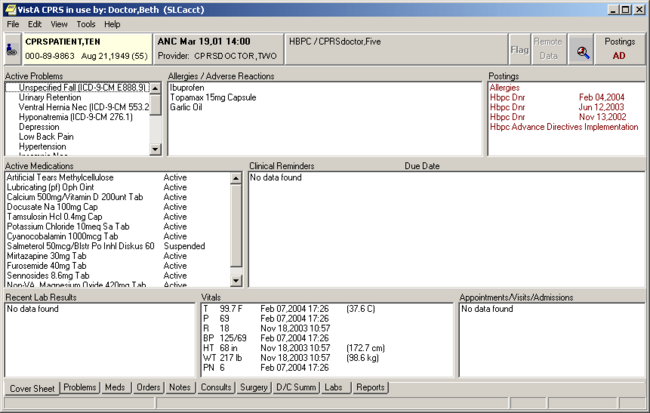
Overview
CPRS enables clinicians to enter, review, and continuously update all order-related information connected with any patient. With CPRS, you can order lab tests, medications, diets, radiology tests and procedures, record a patient's allergies or adverse reactions to medications, request and track consults, and enter progress notes, diagnoses, and treatments for each encounter, and enter discharge summaries. Close integration with the Clinical Reminders and Text Integration packages allows better record keeping and compliance with Clinical Guidelines and medical record requirements.
CPRS not only allows hospital personnel to keep comprehensive patient records, it also enables clinicians, managers, and QA staff to review and analyze the data gathered on any patient in a way that directly supports clinical decision-making..
CPRS Cover Sheet Example
CPRS: Adverse Reaction Tracking
Overview
The Adverse Reaction Tracking (ART) program provides a common and consistent data structure for adverse reaction data. This module has options for data entry and validation, supported references for use by external software modules, and the ability to report adverse drug reaction data to the Food and Drug Administration (FDA).
Features
- Documents patient allergy and adverse drug reaction data.
- Provides the functionality for other VistA modules to extract and add patient reaction data.
- Provides a reporting mechanism that supports VHA Directive 10-92-070 which specifies reporting of adverse drug reactions to the FDA.
- Includes ART event points in an Application Programmers Interface (API) allowing other VistA packages to know when specific ART events take place so package tasks can be performed.
- Alerts the Pharmacy and Therapeutics Committee each time the signs/symptoms are modified for a patient reaction.
- Generates progress notes. Displays all information at the time of an ART event on the Progress Notes API and allows editing of the note prior to sign off.
- Allows the site to track whether the patient has been asked if he/she has allergies.
- Tracks when the patient chart and ID bands have been marked indicating a particular reaction.
- Differentiates between historical and observed reactions.
- Tracks the particular signs/symptoms for a reaction.
- Allows for configuration of allergy files.
- Allows for editing and verification of reaction data.
- Allows for the addition of comments for each reaction to ensure completeness in reporting.
- Contains extensive reporting capabilities.
- Contains an online reference guide.
CPRS: Authorization/Subscription Utility (ASU)
Overview
The Authorization/Subscription Utility (ASU) provides a method for identifying who is authorized to perform various actions on clinical documents. These actions include signing, co-signing, and amending. ASU originated in response to Text Integration Utilities' document definition needs. Current security key capabilities were unable to efficiently manage the needs of clinical documentation (Discharge Summaries, Progress Notes, etc.).
Features
- Defines, populates, and retrieves information about user classes. User classes can be defined hospital-wide or more narrowly for a specific service and can be used across VistA to replace and/or complement keys.
- Links user classes with Text Integrated Utilities (TIU) document definitions and document events.
- Allows sites to maintain membership of users in User Classes and to distribute such maintenance tasks.
- Lists class members as active or inactive.
- Allows infinite hierarchies of subclasses.
- Defines business rules to further manage document activities.
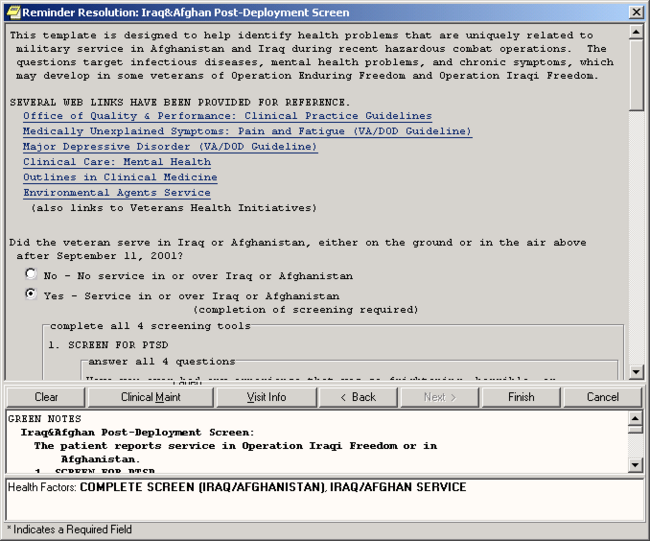
CPRS: Clinical Reminders
Overview
The Clinical Reminders package is a valuable aid in patient treatment. Reminders assist clinical decision-making and educate providers about appropriate care. Electronic clinical reminders also improve documentation and follow-up, by allowing providers to easily view when certain tests or evaluations were performed and to track and document when care has been delivered. They can direct providers to perform certain tests or other evaluations that will enhance the quality of care for specific conditions.
Clinical Reminders may be used for both clinical and administrative purposes. However, the primary goal is to provide relevant information to providers at the point of care, for improving care for veterans. The package benefits clinicians by providing pertinent data for clinical decision-making, reducing duplicate documenting activities, assisting in targeting patients with particular diagnoses and procedures or site-defined criteria, and assisting in compliance with VHA performance measures and with Health Promotion and Disease Prevention guidelines.
The Quality Enhancement Research Initiative (QUERI), a Health Services Research and Development (HSR&D) program, and the National Clinical Practice Guidelines Committee have joined with the Office of Information, System Design & Development office (SD&D) in designing national reminders and dialogs that will help promote informed decision-making and consistency of health care practices. Cooperatively developed reminders include: Ischemic Heart Disease (IHD), Major Mood Disorder (MDD), Hypertension, Iraq and Afghan Post-Deployment Screen, Race and Ethnicity, Women's Veterans Health, My HealtheVet, and VA Geriatric Care Referral (GEC) reminders.
Version 2 of Clinical Reminders contains many enhancements to improve processing and management of reminders. Performance has been enhanced through the creation of an index of all clinical data used in reminder findings. All enhancements are intended to help the Reminders functionality smoothly transition to CPRS Reengineering.
Features
- Allows results that are unique for each patient, by basing reminder evaluation on the patient's clinical data.
- Allows clinicians to resolve reminders through dialogs within the CPRS GUI. Using point-and-click techniques, a clinician can generate text for progress notes, update current and historical encounter data in Patient Care Encounter (PCE), update vital signs, update mental health test results/scores, and place orders.
- Allows facilities to copy, create, and customize their own reminder definitions, based on local needs.
- Provides components that can be displayed on Health Summaries.
- Provides reminders reports for summary or detailed level information about patients' reminders that are due. Reports allow providers to verify diagnoses, verify that appropriate treatment was given, identify patients requiring intervention, and validate effectiveness of care. Combined reports for multiple facilities or multiple locations can now be generated.
- Provides an enhanced Exchange Utility that allows exchange of reminder definitions and dialogs among sites and Veterans Integrated Service Networks (VISNs).
Clinical Reminders Example: Reminders Resolution Dialog
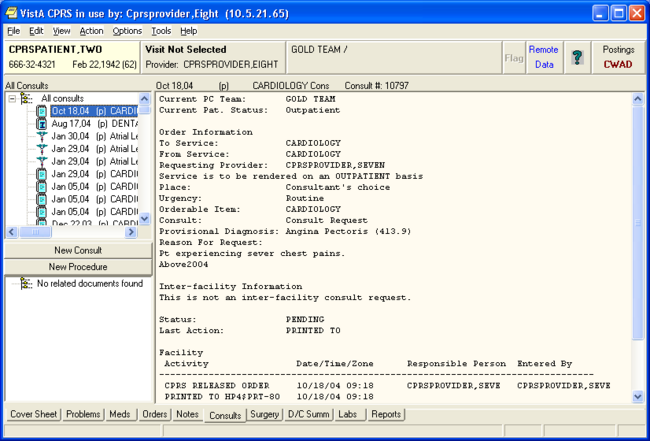
CPRS: Consult/Request Tracking
Overview
The Consult/Request Tracking package provides an efficient way for clinicians to order consultations and procedures from other providers or services within the hospital system, at their own facility or another facility. It also provides a framework for tracking consults and reporting the results. It uses a patient's computerized patient record to store information about consult requests.
Features
- Allows direct access to Consults functions through menu options in CPRS.
- Uses Consults' own menu options for managing the system, generating reports, tracking consults, or entering results for an existing consult request.
- Allows staff to set up consults as CPRS Quick Orders, streamlining the ordering process.
- Integrates with Prosthetics to track Home Oxygen, Eyeglasses, Contact Lenses, and other Prosthetics services.
- Produces a permanent record of the request and resolution for the patient's medical record.
- Allows all relevant parties to see the consult report in the context of the patient's record.
- Allows use of TIU templates and boilerplate to report findings.
- Allows display of Consult reports through TIU and CPRS.
- Enables clinicians to order a consult at another facility, using HL7 Messaging and the VA Intranet.
CPRS: Consult/Request Tracking - continued
Consults Example
CPRS: Health Summary
Overview
A Health Summary is a clinically oriented, structured report that extracts many kinds of data from VistA and displays it in a standard format. Health summaries can be printed or displayed for individual patients or for groups of patients. The data displayed covers a wide range of health-related information such as demographic data, allergies, current active medical problems, and laboratory results.
Features
- Integrates data from the following packages:
Adverse Reaction Tracking Nursing (Vital Signs)
Automated Medical Information Outpatient Pharmacy
Exchange (AMIE) Patient Care Encounter (PCE)
Clinical Reminders Problem List
Computerized Patient Record Progress Notes
System (CPRS) Radiology
Consults/Request Tracking Registration
Dietetics Scheduling
Discharge Summary Social Work
Inpatient Medications Spinal Cord Dysfunction
Laboratory System Surgery
Medicine VistA Imaging
Mental Health
- Health Summary users can print an Outpatient Pharmacy Action Profile with bar codes in tandem with a health summary.
- Health Summary now exports components that allow staff to view remote patient data through CPRS. Additionally, remote clinical data can be viewed using any Health Summary Type that has an identically named Health Summary Type installed at both the local and remote sites.
- Clinical Reminders work with Health Summary to furnish providers with timely information about their patients' health maintenance schedules. Providers can work with local coordinators to set up customized schedules based on local and national guidelines for patient education, immunizations, and other procedures.
- Health Summary components 'Progress Notes' and 'Selected Progress Notes' can display the new interdisciplinary progress notes and all of the entries associated with the interdisciplinary note.
Health Summary Example
CPRS: Problem List
Overview
Problem List is used to document and track a patient's problems. It provides the clinician with a current and historical view of the patient's health care problems across clinical specialties and allows each identified problem to be traceable through the VistA system in terms of treatment, test results, and outcome.
This application supports primary care givers, such as physicians, nurses, social workers, and others, in inpatient and outpatient settings. It is also designed to be used by medical and coding clerks. A variety of different data entry methods are possible with this application.
Use of Problem List varies from site to site, depending on the data entry method a facility has chosen. Many sites use Encounter Forms, with clerks entering most of the data in the encounter forms. Encounter forms are generated from patient data in the system and added to or modified by clinicians.
Features
- Allows a clinician to view an individual problem list for any given patient.
- Supports a variety of specialized views of a patient's problem list.
- Uses the Lexicon utility that permits the use of "natural" terminology when selecting a problem. Each term is well defined and understandable. A user, site, or application may substitute a preferred synonym.
- Can be linked to other sections of the medical record, such as Health Summary, Progress Notes, Order Entry/Results Reporting, Consults, test results, care plans for Nursing and Mental Health, Discharge Summaries, and Billing/Encounter Forms.
- Supports import of problem information from other clinical settings outside the immediate medical facility.
- Allows reformulation of a problem.
- Supports multiple forms of data capture: direct clinician entries, clerk entry, encounter forms, foreign problem lists, scanned encounter forms, hand-held devices, etc.
- Requires minimal data entry.
CPRS: Text Integration Utilities (TIU)
Overview
Text Integration Utilities (TIU) simplifies the use and management of clinical documents for both clinical and administrative medical facility personnel. In connection with Authorization/Subscription Utility (ASU), a facility can set up policies and practices for determining who is responsible or has the privilege for performing various actions on required documents.
The Version 1.0 release included Discharge Summary and Progress Notes. With the release of
CPRS and Consults/Request Tracking, TIU has been upgraded to integrate with these packages.
Features
- Provides boilerplate functionality for the automatic fill-in of information from VistA files into TIU documents. Boilerplates and embedded objects can be set up for specific types of documents for specific clinical needs.
- Interfaces with the Computerized Patient Record System (CPRS): the template utilities in the GUI version of CPRS allow speedy point-and-click composition of notes, consults, and summaries. Templates can be set up for specific types of documents for specific clinical needs. Interfaces with Problem List, Automated Information Capture System (AICS), Patient Care Encounter (PCE), Authorization/Subscription Utility (ASU), Incomplete Record Tracking, Health Summary, and Visit Tracking. Uses a standardized and common user interface, which allows clinicians and others to retrieve many kinds of documents from a single source.
- Enables healthcare practitioners to enter interdisciplinary notes regarding a single episode of care for a patient. This is accomplished through the addition of a level to the tree structure where a note can have children (subordinate entries) and each of the children can have a different author. This provides for more complete patient records and facilitates input from a variety of practitioners regarding a single episode of care.
- Interfaces with VistA Imaging allowing clinicians to link TIU documents to all types of clinical images such as X-rays, MRIs, and CAT scans.
- Uses an integrated database, which lets clinicians, quality management staff, researchers, and management search for and retrieve clinical documents more efficiently because documents reside in a single location within the database.
- Permits document input from a variety of data capture methodologies such as transcription, direct entry through CPRS or the TIU package, or upload of ASCII formatted documents into VistA.
- Uses a uniform file structure for storage of documents and management of document types.
- Uses a consistent file structure for defining elements and parameters of a document.
- Allows a variety of user actions, such as entry, edit, electronic signature, addenda, browse, notifications, etc.
- Allows a variety of management functions, including amendment, deletion, and identification of signature surrogate, re-assignment, and administrative authentication.
- Follows HL7 interface and other communication standards.